Funding freeze on for new facilities as IHA moves primary care into households: Cusden
The best way to improve health care delivery in Nelson is not by enhancing its health care facilities, but by keeping potential patients in their homes, says the interim health service administrator for the Interior Health Authority.
Jane Cusden told city council on Monday that the IHA directive for the mostly rural service region — which includes Nelson — is under its primary community care model, one which is preventative in nature, treating people in their homes before they need a hospital.
“We know that home is best. We know that people want to be home from birth to death,” she said during her annual IHA strategy and pressures presentation to council.
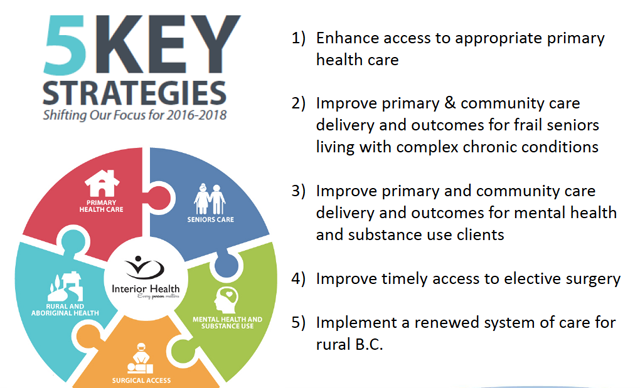
The model forms the first point in a five-point strategy IHA is implementing for the coming year: to enhance access to appropriate primary health care.
Any further funds invested next year will be in community primary care and not in hospitals, she said.
Cusden said the IHA is looking at how physicians treat patients in their offices and how that links in to the emergency department, and how health care can provide “one-stop” medical shops for people.
“The primary care home philosophy is really around what can we provide in the physician’s offices, or easy access to the physicians, so that the family doctors can really manage their patients with care,” she explained.
“People come through to the emergency room because they cannot get appointments. So it’s really a question of how do we make that access for appointments for physicians better.”
Cusden said the IHA is trying to figure out how to support the rural physicians to give them the ability to provide adequate care so patients don’t have to travel too much. In some places the primary care paramedic pilot program is being developed, meaning trained paramedics can travel and deliver primary care to the patients in their own homes.
“They will still have the emergency service, but they will be another level of primary care in the community,” Cusden noted.
One of the IHA strategy points was to renew a system of care for rural B.C., said Mayor Deb Kozak. She wondered what that meant for Nelson.
“I know a lot of the emphasis in most recent time has been on the major centres, acute care hospitals and building new facilities in the bigger centres, but in our area, especially in the Kootenays, we are fairly sparsely populated but we still need good health care,” Kozak said. “So what are some of the strategies being employed to bring that priority to life?”
Cusden pointed to the primary care model as the strategy for Nelson.
“That is really around … having the supports there so that people will get their health close to home and they won’t have to come in to the hospital,” she said.
The IHA also wants to work with community services to support people in their own home with health care.
“If you do the prevention bit, plus the support of people in their own home, we hope we will keep people out of the hospital,” Cusden said. “We can get people home sooner from hospital with those supports.”
That is the shift that is taking place with the IHA, she added, from acute care in the hospitals into primary community care, looking at initiatives that can support that practice.
Currently Kamloops, Kelowna and Grand Forks are piloting the primary care model, with New Denver and Nakusp on the radar. Tele-health is also another area the IHA is looking at increasing so people don’t have to travel to come in to the hospital for an appointment.
“So when you add all of these things up, we are taking patients away from the hospital so the only people that end up in the hospital are people that are really sick that need that higher level of care,” Cusden said.
Coun. Robin Cherbo wondered if the area had enough housing for seniors going into assisted living care, or was there a significant wait list.
“I think there is a wait,” Cusden said, noting she was not sure of the exact residential wait times in Nelson at the moment.
“But the main thing that we really need to do is help people maintain their independence at home,” she added.
“We have waits, but I think there is a lot we can do to preempt people having to go into residential and maintaining them at home.”
Cusden said the IHA looked at how to deliver care across the health care region, and developed five key strategies.
“These are really the focus areas of Interior Health,” she said.
People are living longer, medical conditions are more complex but not necessarily acute, Cusden said, and home is where they want to live, from birth to death.
The second strategy is to improve primary and community care delivery and outcomes for frail seniors living with complex chronic conditions. It means having the service nearest to home.
The third strategy is to improve primary and community care outcomes and delivery for mental health and substance use clients.
“There’s a lot of planning and review of mental health services going on at the moment, and I think that is going to bear great fruit in the future,” Cusden noted.
The fourth strategy is to improve timely access to elective surgery. The IHA has targeted dropping the wait times from 40 to 26 weeks by the end of the next year.
“We are pretty well on target for anyone needing surgery this year will have received it in 40 weeks,” Cusden said.